Abstract
Purpose
To report a rare case of Inverting Papilloma originating from the Lacrimal Sac in Tertiary Hospital.
Method
Case report.
Results
Inverting papilloma is uncommon in lacrimal sac. More often presents in Maxillary sinus, Ethmoid sinus and lateral wall of nasal cavity. This case of 69 years old, Filipino male, who presented with a two-year history of gradually enlarging left medial canthal mass, and tearing. There were no ophthalmoplegia, visual disturbances, proptosis or pain but there was globe displacement superolaterally. Other ophthalmologic examinations were unremarkable at that time of examination. Orbital CT-scan revealed: Heterogenously enhancing mass extending to ipsilateral nasolacrimal canal and nasal cavity causing mass effect. There was note of a suspicious area of hyperostosis. Patient was referred to the Department of Otolaryngology Head and Neck Surgery for co-management. Punch biopsy was done and histopathology revealed Inverting papilloma. Combined surgical management of anterior Maxillectomy via lateral Rhinotomy approach and Dacryocystectomy was done. Intraoperatively, there was note of adhesions to bone in the area of the Lacrimal Sac corresponding to the area of hyperostosis on CT-scan. Post-operative recovery was unremarkable with unchanged visual acuity and extraocular muscle movement.
Conclusions
This is a case of an inverting papilloma involving the lacrimal sac and nasolacrimal duct that was managed with combined anterior maxillectomy via Lateral Rhinotomy approach and dacryocystectomy for complete resection. We recommended complete resection of the tumor to minimize recurrence. Origin in the Lacrimal Sac area was confirmed by intraoperative findings which correlated with CT- scan findings.
Author Contributions
Academic Editor: Shaodan Zhang, Department of ophthalmology, the fourth peoples' Hospital of Shenyang, Shenyang Key Lab of ophthalmology, liaoning, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Elaine Marie Y. Omana, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Inverting Papillomas of the lacrimal sac are rare. The tumor usually originates in the mucosal lining of nasal cavities and paranasal sinuses. It can invade the orbit because of its close proximity. Those that invade the orbit usually present as a medial canthal mass and can cause lacrimal duct obstruction, proptosis, ocular and periorbital pain and diplopia. The nasolacrimal system can be secondarily involved by local extension along the nasolacrimal bony canal or bony erosion with extension through the nasolacrimal system.1,2,4
Primary involvement of the lacrimal sac in inverting papilloma is rare; there are only seven (7) reported cases in literature. We present the eight (8th) case that is from lacrimal sac to be reported with orbital extension.1
This is a case of a 69 year old, Filipino male, who presented with a two-year history of gradually enlarging left medial canthal mass, yellowish eye discharge, tearing and swelling at the left canthal area which did not improve upon administration of antibiotics. The patient had no history of trauma. There were no ophthalmoplegia, visual disturbances, proptosis, pain, epistaxis, rhinorrhea and difficulty of breathing.
A year prior to consultation, the patient noted increase in size of the mass with globe displacement superolaterally that prompted consult with an oculoplastic subspecialist.
The patient is a known hypertensive and had total thyroidectomy 29 years ago for follicular adenoma. Systemic examination did not show any lymphadenopathy or palpable mass in other parts of the body.
Ophthalmologic examination revealed a 20x20 mm firm and fixed mass at the left medial canthal area with globe displacement superolaterally [Figure 1a].
Figure 1a.Pre-Operative picture of patient presenting with left medial canthal mass and globe displacement superolaterally. Figure 1b and 1c. Picture of patient 6 weeks post op.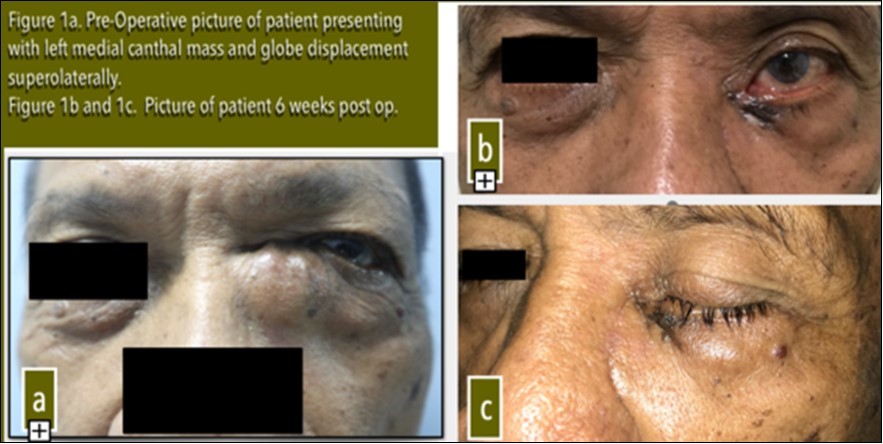
Visual acuity, slit lamp examination, extraocular eye muscle movements were unremarkable at the time of examination except for lacrimal apparatus irrigation which showed blockage at the level of the left common canaliculus. Orbital CT-scan revealed: Heterogenously enhancing mass extending to ipsilateral nasolacrimal canal and nasal cavity causing mass effect. No bone erosions present. There was note of a suspicious area of hyperostosis in the area of the lacrimal sac [Figure 2]. Patient was referred to the Department of Otolaryngology Head and Neck Surgery for co-management. Punch biopsy was done and histopathology revealed Inverting Papilloma.
Figure 2.Orbital CT scan ( 2a Axial. 2b Coronal cuts): Heterogenously enhancing mass at the region of the left inner canthus extending to the ipsilateral nasolacrimal canal and nasal cavity causing mass effect. Encircled is the suspicious area of hyperostosis.
The lesion was completely excised by combined surgical management of anterior maxillectomy via lateral rhinotomy approach and dacryocystectomy [Figure 3a and Figure 3 b]. Intraoperatively, there was note of adhesions to bone in the area of the lacrimal sac corresponding to the area of hyperostosis on CT-scan. Drilling of bone in this area was done to prevent possible recurrence.
Figure 3.a. Combined anterior maxillectomy via lateral rhinotomy and dacryocystectomy exposing the lacrimal sac mass (arrow). b. Surgical specimen of the mass. Upper portion is at the area of the lacrimal sac then the inferior portion is at the inferior turbinate area.
Histopathology results showed tissue fragments lined by squamous and respiratory epithelium with prominent downward endophytic growth of epithelial nests with intact basement membrane conclusive of Inverting Papilloma [Figure 4a, 4b, 4c and 4d].
Figure 4.Lacrimal Sac area. a. Low Magnification x4. Haematoxylin and eosin stained sections of the tumor disclose tissue with prominent downward endophytic growth of round to elongated interconnected epithelial nests lined by squamous and respiratory type of epithelium into the underlying connective tissue stroma forming large clefts and islands. (b) High power Magnification, x40 shows multilayered epithelium. (Arrows)
Post-operative recovery was uneventful with unchanged visual acuity and extraocular muscle movement. Patient was asymptomatic but exhibited mild ectropion [Figure 1b].
Discussion
Inverting papillomas are neoplasms of surface epithelium with fingerlike projections that are locally aggressive in nature. Most inverting papillomas arise in lateral nasal wall but also in lacrimal sac in rare cases. Both may invade the orbit and may present with lacrimal duct obstruction, exophthalmos,periorbital pain, diplopia, medial canthal mass and decreased visual acuity.4Medial canthal mass is the commonest presenting symptom, followed by epiphora which are both present in our patient.1,2,4As of this writing, there are only seven (7) reported cases worldwide of inverting papilloma arising from the lacrimal sac 1.
It is important to determine the area of origin by CT scan to optimize the proper surgical management and prevent recurrence.3Lee et al in his paper in 2007 noted that there is a high correlation between the origin of the inverted papilloma and focal hyperostosis on CT scan which might facilitate prediction of tumor origin.3
In our patient, hyperostosis was noted in the area of the lacrimal sac on CT scan which was clinically correlated intraoperatively with adhesion of the mass to the bone in the lacrimal sac. This is further evidence that the origin of this tumor is in the lacrimal sac.
Surgical excision with clear margins remains the mainstay of the treatment for inverting papilloma of the lacrimal sac. Further resection of bone at the area of attachment may prevent recurrence. Those invading the orbit as in our case, where there is already extension to the nasolacrimal apparatus and displacement of the globe, necessitate a combined surgical approach of anterior maxillectomy with dacryocystectomy.
There is a good long term term prognosis for complete excision with clear margins of inverting papillomas. Recurrence rate of 14% in lacrimal sac compared to nasal and paranasal sinus inverting papillomas which has 10-34% recurrence rate.1
Conclusion
Inverting Papilloma is a rare disease most especially arising from the lacrimal sac. A 69 year old Filipino male presenting with left medial canthal mass underwent combined anterior maxillectomy via lateral rhinotomy approach and dacryocystectomy. Histopathology revealed Inverting Papilloma.
Focal hyperostosis on CT scan and intraoperative findings of adhesions highly suggest origin of this tumor to be in the lacrimal sac.
References
- 1.Hardy A W, Dwivedi R C, Masterson L, Riffet F, Marker A et al. (2015) Inverted papilloma of lacrimal sac invading into orbit: Case report and review of literature. , J Can Res There 11, 238-40.
- 2.Chaudhry I A, Taiba K, Al-Sadhan Y, Riley F C.Inverted papilloma invading the orbit through the nasolacrimal duct: A case report.
