Abstract
This evidence-based brief commentary discusses the potential of EPIC ® medicalrecords software to help or hinder in advancing High Reliability in healthcare—namely, the intent to attain repeatable, increasingly high levels of quality and safety over time. Four of EPIC’s key aspects relevant to High Reliability are examined: Standardized (High Quality) Information / Data Collection, Technological Somnambulism, Enhanced Patient Safety, and Reminders / “Hardstops.” A conclusion is drawn that EPIC, if used correctly, has vast potential to advance High Reliability high-quality and safety, specifically in medical treatment and regarding healthcare organization practice in general. However, it has hidden costs that are more than money; if unfettered, those costs can hinder its usefulness and even render it counterproductive. EPIC only works well in terms of Maximum High Reliability in healthcare as long as users and leaders remain mindful, prudent, and balanced in its use.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2024 Ralph J. Johnson
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
High incidence rates of preventable patient harm represent a substantial expense for healthcare organizations—not only fiscally but in terms of public perceptions of their ability to deliver high-quality and safe healthcare.1 High-quality healthcare and patient safety has always been a paramount, quintessential and ubiquitous concern and the subject of increasing attention from healthcare leaders.1, 2 Healthcare organizations are responding by incorporating quality and safety initiatives into their processes and planning.1, 2 As such, they have been adopting the concept and processes of High Reliability.3
High Reliability was developed by researchers studying other organizations fraught with potential risk, error, hazards, and failures, e.g., commercial aviation and nuclear power, that operated under similarly precarious circumstances as the healthcare field; nevertheless, they have maintained consistently high quality and safety levels that far exceed those of healthcare organizations.1, 2, 3 Logically, adapting and practicing the lessons learned regarding High Reliability offers the potential for healthcare organizations to achieve comparable quality and safety.1, 2
High Reliability is a persistent “mindfulness” or “awareness” with the intent to attain increasingly high levels of quality and safety over time in all service delivery contexts.1 The commonly accepted definition of High Reliability refers to any culture that aims at reducing error incidence and improving quality/safety to acceptable levels in every procedure or process every time while operating in complex, high-risk, hazardous arenas (e.g., hospitals, clinics, healthcare organizations).1, 2, 3 Research has found a relationship between healthcare organizations who hardwire specific High Reliability tools, behaviors, and processes; promote redundancy and repetitiveness in their organizational culture; and ensure and maintain high quality and safety.3
High Reliability in healthcare organizations not only entails constant, repetitive standardization to advance high quality and safety, but also entails a comprehensive and adaptive approach to reduce incidents, failures, and harm. 2, 3 Many healthcare organizations are undertaking High Reliability initiatives with varying results.1
A keystone to successful implementation of High Reliability initiatives in healthcare is efficient and compliance access to appropriate patient health records data and information, while balancing science and speed to convert that into evidence upon which to base best practices.1, 2, 3 For healthcare organizations, there are certified, off-the-shelf, one-resource, electronic information and research systems that have become popular choices.4 Also, this is due to government mandates for the adoption of “meaningful use” health records software that offers varying levels of potential to inform and promote High Reliability-esque initiatives in patient medical treatment and healthcare organization decisions.5 The choice for many healthcare organizations is EPIC ®, which has seemingly become iconic, emblematic, and synonymous with meaningful-use healthcare records software management; EPIC has garnered > 30% of the EHR market shares while seeking market shares in other industries.4, cf.5
Thus, it is sensible to address EPIC’s aspects that are ostensibly relevant to advancing High Reliability in healthcare, specifically: Standardized (High Quality) Data Collection; Technological Somnambulism; Enhanced Patient Safety; and Reminders and “Hardstops.”4 Despite EPIC’s increasing prominence, information technology, and a logical gravitation toward High Reliability in healthcare, there are few if any treatments in the literature considering aspects surrounding its meaningful-use features and their relevance to High Reliability.cf. 4, 5 Therefore, the intent of this brief commentary is to close that gap and consider the relevance of aspects surrounding its meaningful-use features in support of High Reliability in healthcare. Though this brief commentary solely considers EPIC, the considerations reported herein may be similarly reflective of other similar, certified meaningful-use electronic records software since meaningful-use criteria and High Reliability are mandated by law.6
Standardized (High Quality) Information / Data Collection
A benchmark of High Reliability in healthcare is the ability to deliver intelligent, efficient, consistently structured, automated, mindful, and sustainable data—which EPIC provides.6, 7, 8 High Reliability in healthcare seeks readily reproducible and efficient coordination of high-quality and safe medical treatment through programmed auto-connectivity and comparable information / data, especially patients’ records—which EPIC also provides.6, 7, 1, 2, 3. EPIC can generate accurate and timely reports based on its internal requirements for standardized data entry (e.g., “Hardstops”—data entry does not move until they are addressed).10, 11, 12, 13, 14 This can be immediately queried in the form of high-quality readable reports for purposes of programmatic evaluation and responsive modification to address potential safety risks, hazards, and failures.10, 15, 16 That is, EPIC allows for mindful and purposeful modification within a structured format with the inclusion of prompts and Hardstops for the collection of mandatory relevant entry of safety data.17, 18, 19, 20, 21, 22
Though reasonably malleable and responsive, EPIC’s structured and standardized data-ready features can be leveraged to target and track medical procedures and processes to enhance successful high-quality care and proactively reduce safety risks, hazards and failures while incrementally improving cost-effective medical and healthcare organizational decisions based on empirically-derived best practices. 17, 18, 23, 24, 25, 26
A key to High Reliability in healthcare is alertness to high quality and risk avoidance, and seeking cost-effectiveness and efficiency. These trigger the marshalling of substantial amounts of data, which EPIC affords.10, 27 EPIC can be conformed to shepherd data entry and pre-identify errors, hazards, and failures and threaded patterns; these can be derived from nearly at the point of clinician entry.28, 29, cf. 9 Thus, relevant data can be readily identified almost in real time, enhancing accuracy and high quality of data as well as informing adjustments of medical service performance so as to enhance quality and safety.20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38
Technological Somnambulism
Structured and standardized data entry come at a potential price; specifically, a tendency toward reflexive, non-reflective, and non-mindful technology-driven hypnosis that can to some extent be described as “sleepwalking.”39, 40, 41 That is, front-end data collection is shepherded through heavy reliance on pre-ordained (i.e., “canned”) forms and templates that can be narrow, rigid, and unchanging versus purposefully produced, truly meaningful information. 42 The remedy is to make the forms and templates reflectively responsive and mindful. This can be done using dedicated teams of health experts and software engineers and sub-vendors to update, adapt, customize and include modified forms and templates through the medical care cycle—but all that comes at a heavy expense.28, 42, 43, 44 cf. 45
Regarding this drawback, a similar downside in terms of High Reliability in healthcare is that EPIC tends to discourage entry of more specific and detailed information, except with expensive modifications and add-ons that diminish overall efficiency.46, 47, 48, 49, 50, 51 Since product development is regulated—and for that reason alone—it can be a lengthy process and expensive.52, 53 Put differently, in terms of High Reliability in healthcare, EPIC is a powerful tool for monitoring constant adherence to high-quality production / process and safety best practices—but ironically, only with a potential, if left unchecked, for sacrificing a degree of mindfulness, workflow efficiency, and cost-effectiveness. The rub is achieving effective balance. cf. 54
Enhanced Patient Safety
A plus in terms of High Reliability for EPIC is its explicit aim of improving patient safety through accurately deriving outcome measures that are vital for identifying and addressing potential risks, hazards, failures and related patterns.7 EPIC’s ability to standardize and auto-connect data helps inform and accelerate patient recoveries as well as avoid medical errors, thus enhancing and routinizing high-quality and safe evidence-based practices and cost-effective preventive medicine.18, 52, 55, 56, 57 Also, EPIC provides interoperability and interconnectivity, permitting routine ease of follow-ups pursuant to continuity of care and safety—consistent with the concept of High Reliability in healthcare.7, 58, 59, 60, 61, 62, 63, 64 6566 In other words, an upside for EPIC in terms of High Reliability in healthcare is that EPIC derives and reports comprehensive information / data almost in real time, helping to identify patient risks. This lends itself to excellent patient tracking, monitoring, and follow-up, while documenting preventable complications, risks, and sources for dangerous unplanned outcomes. 7, 9, 24, 42
Reminders / Hardstops
A central feature of EPIC that, if left ungoverned by mindfulness, can detract from its ability to support High Reliability, is its “Reminders” and “Hardstops.42, 67, 68, 69 Specifically, users must address these successfully before proceeding with data entry. That interrupts and disturbs steady workflow, quickly erodes users’ mindfulness, and has been reported to diminish EPIC’s usefulness in entering data with which to ensure high-quality and safety; also, it diminishes basic alertness to matters of repeatable best practices, risk avoidance, and preventive medicine.37, 70, 71, 72 Simply put, clinicians are too busy struggling with data entry to bother with anything else. Clinicians can soon become overwhelmed and overburdened with treatment advisories and disruptive documentation requirements.62, 71
Research has shown marked improvements in end users’ work if prudent limits are placed on Reminders and Hardstops.39 Reminders and Hardstops, when installed properly and used mindfully, substantially improve clinician compliance in terms of data entry rates and requirements for documentation and a dherence to safe and high-quality treatment regimes.39, 40, 41 This is why Reminders and Hardstops (as well as standardized templates) probably work better than relying on haphazard and disorganized passive entry in terms of measuring outcomes and improving quality and safety.39, 40, 41 However, if allowed to proliferate unfettered, Reminders and Hardstops can literally transform clinicians into overworked data entry clerks, which can become quite burdensome, time-consuming, and disaffecting.17, 71, 72, 73, 74 The takeaway is that installation of Reminders and Hardstops must be clearly justified in terms of value add and necessity in the interest of advancing high quality and safety. 7, 75
Discussion / Conclusion
The commentary herein reported on aspects surrounding EPIC’s meaningful-use features relevant to supporting High Reliability in healthcare—that is, their ability for quickly, efficiently, and repeatedly informing and enabling high quality and safety in healthcare processes, decisions, and patient treatment. This commentary noted that EPIC provides a strong, solid, structured, front-end-to-back-end system for rapid healthcare data collection and auto-interconnected management and retrieval of medical records and information. This lends itself to rapid reporting and informing High Reliability initiatives, decisions, and processes in healthcare. As such, it has vast potential to advance High Reliability high quality and safety, specifically in medical treatment and generally in healthcare organizational practices.
Nonetheless, that potential is achieved with hidden costs. Its structured and standardized format promotes reflexive, non-reflective, and non-mindful situations where the computer is doing all the driving and thinking and becomes an end in itself. Moreover, unfettered and unlimited Hardstops and Reminders and various extensions and add-ons can increase workloads on clinicians. If unchecked, this results in increasing inefficiencies and non-mindfulness, and again the computer can become an end in itself. Ironically, both scenarios can detract from High Reliability in healthcare and ultimately high quality and safety—and both scenarios could occur simultaneously. This is not to mention potentially pricey add-ons for special captures, the need for panels of experts and software engineers, and the lengthy and expensive process all that may entail. The question is: At what point are there diminishing returns and how can organizations achieve a delicate yet efficacious balance?
EPIC has the incomparable ability and potential to help achieve High Reliability in terms of ensuring continuous high-quality care and patient safety, and responsively informing the adjustment of clinical care accordingly. It does so not only through standardized, comprehensive, comparable, and interconnected data collection, but also through purposeful and worthwhile use of Hardstops and Reminders. Nevertheless, EPIC only works well in terms of High Reliability in healthcare as long as users and leaders remain mindful and prudent (see Figure 1).
Figure 1.Mindfulness Achieves Maximum High Reliability Striking a Delicate Balance between Standardization and Informing High-quality and Safety. *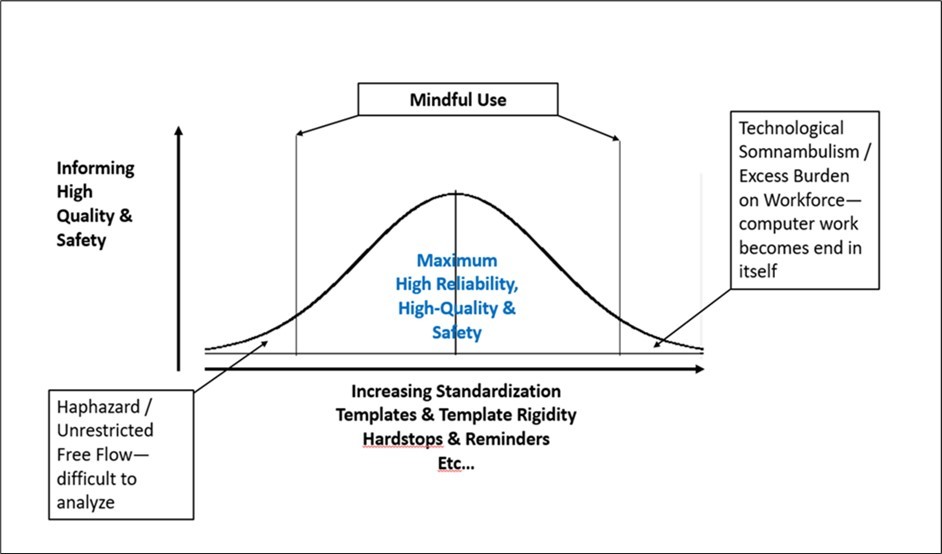
*Note: Bell-shaped Curve CC BY SA gratefully acknowledged.
Figure 1 Illustrates that healthcare leaders / users of EPIC’s meaningful use features must be mindful of striking a delicate balance between standardization and seeking to inform high quality and safety in order to achieve Maximum High Reliability. That is, going too far in any direction will become counterproductive and even harmful.
This report on EPIC’s features and faults regarding High Reliability in healthcare high-quality and safety is mixed. EPIC is probably overall no better or worse than any of its competitors—or any system that uses template regeneration and auto-connect76—because they all strive for the same meaningful use as mandated by federal and state laws. If anything, this commentary reveals that the ultimate price of using meaningful use software in advancing High Reliability in healthcare is eternal mindful use.
Declarations
Ethical approval and consent to participate
Non-applicable, this was a commentary based on open-source documents.
Consent for Publication
Yes.
Availability of data and materials
Yes, “datasets” used and/or analyzed during the current study are available from the corresponding author on reasonable formal request.
Funding
Non-applicable, this research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Authors’ Contribution
Non-applicable, there is one sole Author.
Acknowledgements
The Author wishes to gratefully acknowledge in-kind support of the Department of Lymphoma and Myeloma, UT-MD Anderson Cancer Center, Houston, TX. in the preparation of this manuscript. Also, the author thanks Mr. Jasper Olsem for his encouragement in pursuing the subject matter and proof of concept and Ms. Aileen “Acey” Cho freelance-copy editor for proofing and copyediting drafts. The opinions expressed are solely those of the Author.
Corresponding Author
Reprints and correspondence should be addressed to the author at [email protected], or [email protected], UT-MDACC, Unit 429, 1515 Holcombe, Houston, Texas, 77030-400, U.S.A.. (832-750-1446; 832-372-3511)
References
- 1.Cochrane B S, Hagins M Jr, Picciano G, King J A. (2017) High reliability in healthcare: creating the culture and mindset for patient safety.HealthcManage Forum:. Epub PMID: 28929881https://journals.sagepub.com/doi/epub/10.1177/0840470416689314 30(2), 61-68.
- 2.Chassin M R, Loeb J M. (2013) High-reliability health care: getting there from here.Milbank Q:. 91(3), 459-90.
- 3.Pronovost P J, Berenholtz S M, Goeschel C A, Needham D M. (2006) Creating high reliability in health care organizations.Health Serv Res:. , Aug;41(4 Pt 2, 1599-617.
- 4.Johnson R J. (2021) A comprehensive Research Study Literature Review of EPIC© in terms of enabling Healthcare Agility: A report card. , J Med Informatics Dec Making: 1(4), 1-20.
- 5.Johnson R J. (2016) A Comprehensive Review of an. Electronic Health Record System Soon to Assume Market Ascendancy: EPIC®. JHealthcCommun 1, 10-4172.
- 6.Blumenthal D, Tavenner M. (2010) The “meaningful use” regulation for electronic health records.N Engl JMed:;. 363, 501-504.
- 7.Demirkan H. (2013) Smart healthcare systems framework:. More service oriented, instrumented, interconnected and intelligent.IEEE IT Professional: September/October 38-45.
- 8.Ferris N. (2010) Meaningful Use” of electronic health records.HealthAff::http://www.healthaffairs.org/healthpolicybriefs/brief.php?. 24.
- 9.Katzan I, Speck M, Dopler C, Urchek J. (2011) The Knowledge Program: An innovative, comprehensive, electronic capture system and warehouse.AMIA Ann Symp. Proc. 2011;2011: 683-92. Epub Oct 22. PMID: 22195124 PMCID: PMC3243190https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3243190/ .
- 10.Koppel R, Lehmann C U. (2015) Implications of an emerging EHR monoculture for hospitals and healthcare systems.Am Med Inform Assoc:. 22(2), 465-71.
- 11.Stirling A, Tubb T, Reiff E S, Grotegut C A. (2020) Identified themes of interactive visualizations overlayed onto EHR data: an example of improving birth center operating room efficiency.J Am Med Inform Assoc. 32181803-10.
- 12.Sanelli-Russo S, Folkers K M, Sakolsky W, Fins J J. (2018) Meaningful Use of Electronic Health Records for Quality Assessment and Review of Clinical Ethics Consultation.J Clin Ethics. 29(1), 52-61.
- 13.Milinovich A, Kattan M W. (2018) Extracting and utilizing electronic health data from Epic for research.AnnTranslMed. 10.21037/atm.2018.01.13 PMCID: PMC5879514 PMID: 6(3), 29610734-5879514.
- 14.McDowell J, Wu A, Ehrenfeld J M, Urman R D. (2017) Effect of the Implementation of a New Electronic Health Record. System on Surgical Case Turnover Time.J Med Syst. 2017 Mar;41(3): 42 27, 10-1007.
- 15.Whalen K, Lynch E. (2018) Transition to a new electronic health record and pediatric medication safety: lessons learned in pediatrics within a large academic health system. J Am Med Inform Assoc.:. 25(7), 848-854.
- 16.Feldstein D A, Barata I, McGinn T, Heineman E. (2023) Disseminating child abuse clinical decision support among commercial electronic health records: Effects on clinical practice.JAMIA Open Access. doi: 10.1093/jamiaopen/ooad022. eCollection 2023 Jul. PMID: 37063409 PMCID: PMC10101685https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10101685/pdf/ooad022.pdf 6(2).
- 17.Bornstein S. (2012) An integrated EHR at Northern California Kaiser-Permanente.App Clin Inform:. 3(3), 318-25.
- 18.Heidemann L, Law J, Fontana R J. (2017) A text searching tool to identify patients with idiosyncratic drug-induced liver Injury.Dig Dis Sci. 62(3), 615-625.
- 19.Lindén-Lahti C, Kivivuori S-M, Lehtonen L, Schepel L. (2022) Implementing a new Electronic Health Record System in a university hospital: The Effect on reported medication Errors.Healthcare (Basel). doi: 10.3390/healthcare10061020 PMCID: PMC9222436 PMID: 10(6), 1020.
- 20.Yazdanshenas H, Osias E, Hwang R, Park D Y. (2022) Retrospective evaluation of cervical fusion with DTRAX (R) cervical cage. JCraniovertebrJunction Spine. Jan-Mar; 13(1): 48–54. doi: 10.4103/jcvjs.jcvjs_150_21 PMCID: PMC8978854 PMID: 35386243-8978854.
- 21.Zhang C Q, Gogal C, Gaugler T, lome-Eberwein S. (2021) A 6-Year Experience of Laser Treatments for Burn Scars in a Regional Burn Center-Safety, Efficacy, and Quality Improvement.J Burn Care Res:. 42(1), 74-81.
- 22.Vanneman M W, Balakrishna A, Lang A L, Eliason K D. (2020) Improving Transfusion Safety in the Operating Room With a Barcode Scanning System Designed Specifically for the Surgical Environment and Existing Electronic Medical Record Systems: An Interrupted Time Series Analysis.AnesthAnalg:. Oct;131(4): 1217-1227. doi: 10.1213/ANE.0000000000005084. PMID: 32925343file:///C:/Users/Jayjo/Downloads improving_transfusion_safety_in_the_operating_room.31.pdf .
- 23.Chandiramani A, Gervasio J, Johnson M, Kolek J. (2018) Who's Covering This Patient?' Developing a First-Contact Provider (FCP) Designation in an Electronic Health Record: J Comm Qual PatientSaf. Feb;44(2): 107-113. doi: 10.1016/j.jcjq.2017.08.005. Epub 3, 29389459-1553725017302428.
- 24.DeBoer E M, Prager J D, Kerby G S, Stillwell P C. (2016) Measuring pediatric bronchoscopy outcomes using Electronic Medical Record.Ann AmThoracSoc:. 27, 10-1513.
- 25.Ogita M, Yamashita H, Nozawa Y, Ozaki S. (2021) Phase II study of stereotactic body radiotherapy with hydrogel spacer for prostate cancer: acute toxicity and propensity score-matched comparison:RadiatOncol.Jun 12;16(1):. 107-10.
- 26.Tayefi M, Ngo P, Chomutare T, Dalianis H. (2021) Challenges and opportunities beyond structured datain analysis of electronic health. 13-1549.
- 27.Adelson K B, Qiu Y C, Evangelista M, Spencer-Cisek P. (2014) Implementation of electronic chemotherapy ordering: an opportunity to improve evidence-based oncology care.J OncolPract:. Mar;10(2):e113-9. doi: 10.1200/JOP.2013.001184. Epub .
- 28.Bellon J E, Stevans J M, Cohen S M, James AE 3rd. (2015) Comparing advanced practice providers and physicians as providers of e-visits.TelemedJ E Health:. doi: 10.1089/tmj.2014.0248. Epub 21(12), 1019-26.
- 29.Beck J D, Deegan J H, Riehl J T, Klena J C. (2010) Incidence of scapholunate ligament dissociation in patients with aspiration-confirmed gout.J Hand Surg Am:. 10.1016/j.jhsa.2010.08.009. Epub 35(12), 1938-42.
- 30.Blazevski A, Amin A, Scheltema M J, Balakrishnan A. (2021) Focal ablation of apical prostate cancer lesions with irreversible electroporation (IRE).World JUrol:. 39(4), 1107-1114.
- 31.Finn A, Bondarenka C, Edwards K, Hartwell R. (2017) Evaluation of electronic health record implementation on pharmacist interventions related to oral chemotherapy management.J Oncol PharmPrac:. Epub PMID: 27573921https://journals.sagepub.com/doi/epub/10.1177/1078155216665247 23(8), 563-574.
- 32.Sharpless B R, Del Rosario F, Molle-Rios Z, Hilmas E. (2018) . Use of Electronic Health Record Tools to Facilitate and Audit Infliximab Prescribing. JPediatrPharmacolTher: Jan-Feb;23(1): 18-25.
- 33.Jain V S, Li H, Lee K P, Rose W N. (2023) Therapy plans for therapeutic apheresis in Epic HealthLink.J ClinApher:. Oct;38(5): 611-614. doi: 10.1002/jca.22072. Epub PMID: 37376707https://onlinelibrary.wiley.com/doi/epdf/10.1002/jca.22072 .
- 34.Dinora D R, ElderJ J, Harwood K A. (2021) Design, Implementation, and Evaluation of Compliance With Pharmacy Workflow During a Pediatric Oncology Computerized Provider Order Entry (CPOE). , Launch.JPediatrPharmacolTher: 26(5), 491-496.
- 35.Knake L A, Ahuja M, McDonald E L, Ryckman K K. (2016) Quality of EHR data extractions for studies of preterm birth in a tertiary care center: guidelines for obtaining reliable data.BMCPediatr:. 29, 10-1186.
- 36.McKay K M, Apostolopoulos N, Dahrouj M, Nguyen H V. (2021) Assessing the Uniformity of Uveitis Clinical Concepts and Associated. ICD-10 Codes Across Health Care Systems Sharing the Same Electronic Health Records System.JAMAOphthalmol: 139(8), 887-894.
- 37.Burke P C, Eichmuller L, Messam M, Duffy D A. (2019) Beyond the abacus: Leveraging the electronic medical record for central line day surveillance.Am J Infect Control:. Nov;47(11): 1397-1399. doi: 10.1016/j.ajic.2019.05.013. Epub 2019 Jul 2. PMID: 31278000https://www.sciencedirect.com/science/article/pii/S0196655319305735?via%3Dihub .
- 38.Riley J B, Justison G A. (2015) Perfusion Electronic Record Documentation Using Epic Systems Software. , JExtraCorporTechnol: 47(4), 242-4.
- 39.Langsjoen J, Goodell C, Castro E, Thomas J. (2015) Improving compliance with cervical cancer screening guidelines.Proc. (BaylUniv Med Cent).Oct;28(4): 450-3. PMID: 26424938 PMCID: PMC4569221 DOI: 10.1080/08998280.2015.11929305https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4569221/ .
- 40.Unni S, Yao Y, Milne N, Gunning K. (2015) An evaluation of clinical risk factors for estimating fracture risk in postmenopausal osteoporosis using an electronic medical record database.OsteoporosInt. 26(2), 581-7.
- 41.Hayek S, Nieva R, Corrigan F, Zhou A. (2014) End-of-life care planning: improving documentation of advance directives in the outpatient clinic using electronic medical records.JPalliatMed. Dec;17(12): 1348-52. doi: 10.1089/jpm.2013.0684. PMID: 24988497-10.
- 42.Carberry K, Landman Z, Xie M, Feeley T. (2016) Incorporating longitudinal pediatric-centered outcome measurement into the clinical workflow using a commercial electronic health record: A step toward increasing value for the patient.J Am Med Inform Ass:. 23, 88-93.
- 43.Rameau A, Wang E, Saraswathula A, Natalie Pageler N. (2018) Enhancing pediatric airway safety using the electronic medical record.Laryngoscope:. Dec;128(12): 2885-2892. doi: 10.1002/lary.27261. Epub 8, 30195274-10.
- 44.Klehr J, Hafner J, Spelz L M, Steen S. (2009) Implementation of standardized nomenclature in the electronic medical record.Int JNursTerminolClassif:. 20(4), 169-80.
- 45.Sittig D F, Ash J S, Wright A, Chase D. (2020) How can we partner with electronic health record vendors on the complex journey to safer health care?JHealthcRisk Manag:. Oct;40(2): 34-43. doi: 10.1002/jhrm.21434. Epub 2020 Jul 9. PMID: 32648286https://onlinelibrary.wiley.com/doi/epdf/10.1002/jhrm.21434 .
- 46.Makam A N, Lanham H J, Batchelor K, Samal L. (2013) Use and satisfaction with key functions of a common commercial electronic health record: A survey of primary care providers.BMC Med Inform Decision Making:. 13, 10-1186.
- 47.Sweet K, Gordon E S, Sturm A C, Schmidlen T. (2014) Design and implementation of a randomized controlled trial of genomic counseling for patients with chronic disease.J Pers Med. 4(1), 1-19.
- 48.Cheriff A D, Kapur A G, Qiu M, Cole C L. (2010) Physician productivity and the ambulatory EHR in a large academic multi-specialty physician group.Int J Med Inform. Jul;79(7): 492-500. doi: 10.1016/j.ijmedinf.2010.04.006. PMID: 20478738https://www.sciencedirect.com/science/article/abs/pii/S138650561000095X?via%3Dihub .
- 49.Seltzer A Ramirez-Zohfeld, Xiong L, Morse L, Lindquist L A. (2020) . Use of Electronic Health Records by Older Adults, 85 and Older, and Their Caregivers.J AmGeriatrSoc. Mar 11. doi: 10.1111/jgs.16393. [Epub ahead of print] PMID: 32159860https://onlinelibrary.wiley.com/doi/abs/10.1111/jgs.16393 .
- 50.Mathioudakis N, Jeun R, Godwin G, Perschke A. (2019) Development and Implementation of a Subcutaneous Insulin Clinical Decision Support Tool for Hospitalized Patients.J Diabetes Sci Technol:. Epub 13(3), 522-532.
- 51.Peticolas K, Khairat S, Seashore C, Law J. (2019) Physician-Led EHR Customization Tracking Assessments for Pediatric Patients with Turner Syndrome.Stud Health Technol Inform. 4, 276-279.
- 52.Moreno-Iribas C, Sayon-Orea C, Delfrade J, Ardanaz E. (2017) Validity of type 2 diabetes diagnosis in a population-based electronic health record database.BMC Med InformDecisMak. 17(1), 10-1186.
- 53.Calvitti A, Hochheiser H, Ashfaq S, Bell K. (2017) Physician activity during outpatient visits and subjective workload.J. 10.1016/j.jbi.2017.03.011. Epub , Biomed Inform. May; 69, 135-149.
- 54.Menon S, Singh H, Giardina T D, Rayburn W L. (2017) Safety huddles to proactively identify and address electronic health record safety.J Am Med Inform Assoc:. 24(2), 261-267.
- 55.Grigoryan L, Zaroob R, Wang H, Trautner B W. (2015) Low concordance with guidelines for treatment of acute cystitis in primary care.Open Forum Infect Dis. doi: 10.1093/ofid/ofv159. eCollection. PMID: 26753168 PMCID: PMC4675917https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4675917/ 2(4).
- 56.Carter Z A, Goldman S, Anderson K, Li X. (2017) Creation of an Internal Teledermatology Store-and-Forward System in an Existing Electronic Health Record: A Pilot Study in a Safety-Net Public Health and Hospital System.JAMA Dermatol. 153(7), 644-650.
- 57.Bush R A, Connelly C D, Pérez A, Barlow H. (2017) Extracting autism spectrum disorder data from the electronic health record.Appl Clin Inform. 731-741.
- 58.Ho V T, Klumpp T R, Liang W H, Prestegaard M, Horwitz M. (2023) Cell Therapy Informatics: Updates on the Integration of HCT/IEC Functionalities into an. Electronic Medical Record System in the US to Promote Efficiency, Patient Safety, Research, and Data Interoperability.Transplant Cell Ther: 2023 Sep;29(9): 539-547. doi: 10.1016/j.jtct.2023.06.014. Epub PMID: 37379969https://www.sciencedirect.com/science/article/pii/S266663672301360X?via%3Dihub .
- 59.Jones S, Hislop J L, Gilmore H, Greenway A. (2023) Using an electronic medical record patient portal for warfarin self-management: Empowering children and parents.ResPractThrombHaemost:. 7(2), 100066-10.
- 60.Nikolian V C, Williams A M, Jacobs B N, Kemp M T. (2018) . Pilot Study to Evaluate the Safety, Feasibility, and Financial Implications of a Postoperative Telemedicine Program.Ann Surg: 268(4), 700-707.
- 61.Mershon B H, Vannucci A, Bryson T, Lin F. (2021) A Collaborative Partnership between the Multicenter Handoff Collaborative and an Electronic Health Record Vendor.Appl Clin Inform: . 12(3), 647-654.
- 62.Goudra B, Singh P M, Borle A, Gouda G. (2016) Effect of introduction of a new electronic anesthesia record (Epic) system on the safety and efficiency of patient care in a gastrointestinal endoscopy suite-comparison with historical cohort.Saudi JAnaesth:. 10(2), 127-31.
- 63.Bouhenguel J T, Preiss D A, Urman R D. (2017) Implementation and Use of Anesthesia Information Management Systems for Non-operating Room Locations.AnesthesiolClin:. Dec;35(4): 583-590. doi: 10.1016/j.anclin.2017.07.001. PMID: 29101948https://www.sciencedirect.com/science/article/pii/S1932227517300605?via%3Dihub .
- 64.Bydon M, Goyal A, Biedermann A, IlliesAJC Canoy. (2021) Building and implementing an institutional registry for a data-driven national neurosurgical practice: experience from a multisite medical center.NeurosurgFocus: . PMID: 26677410 PMCID: PMC4681056 51(5), 10-1186.
- 66.Shermock S B, Schepel LL ShermockKM. (2023) Closed-Loop Medication Management with an Electronic Health Record System. in U.S. and Finnish Hospitals.Int J Environ Res Public Health: Aug 30;20(17): 6680. doi: 10.3390/ijerph20176680. PMID: 37681820 PMCID: 10488169-10488169.
- 67.Chi J, Kugler J, Chu I M, Loftus P D. (2014) Medical students and the electronic health record: 'an epic use of time'.Am. Sep;127(9): 891-5. doi: 10.1016/j.amjmed.2014.05.027. Epub 4-0002.
- 68.Ratwani R M, Savage E, Will A, Arnold R, Khairat S. (2018) A usability and safety analysis of electronic health records: a multi-center study. , J Am Med Inform Assoc: 25(9), 1197-1201.
- 69.Pruitt Z, Howe J L, Krevat S A, Khairat S. (2022) Development and pilot evaluation of an electronic health record usability and safety self-assessment tool.JAMIA Open:. doi: 10.1093/jamiaopen/ooac070. eCollection 2022 Oct.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9338455/pdf/ooac070.pdf 5(3).
- 70.Fortman E, Hettinger A Z, Howe J L, Fong A. (2020) Varying rates of patient identity verification when using computerized provider order entry.J Am Med Inform Assoc. 27(6), 924-928.
- 71.Lewinski A A, Drake C, Shaw R J, Jackson G L. (2019) Bridging the integration gap between patient-generated blood glucose data and electronic health records.Stud Health Technol Inform. 4, 276-279.
- 72.Shah S N, Seger D L, Fiskio J M, Horn J R. (2021) . Comparison of Medication Alerts from Two Commercial Applications in the USA.DrugSaf: . 2021 Jun;44(6): 22, 661-668.
- 73.Helmers R, Doebbeling B N, Kaufman D, Grando A. (2019) Mayo Clinic Registry of Operational Tasks (ROOT): A Paradigm Shift. in Electronic Health Reco Implementation Evaluation.Mayo Clin ProcInnovQual Outcomes. Aug 23;3(3): 319-326. doi: 10.1016/j.mayocpiqo.2019.06.004. eCollection 2019 Sep. PMID: 31485570 PMCID: PMC6713835https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6713835/ .
- 74.Seu M, Cho B H, Pigott R, Sarmiento S. (2020) . Trends and Perceptions of Electronic Health Record Usage among Plastic Surgeons.PlastReconstrSurg Glob Open: . Apr 24;8(4):e2709. doi: 10.1097/GOX.0000000000002709. eCollection 2020 Apr. PMID: 32440400 PMCID: PMC7209869https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7209869/pdf/gox-8-e2709.pdf .
Cited by (1)
- 1.Chen Junye George, Lai Hao Xing, Wong Shi Min, Pan Terry Ling Te, Lim Er Luen, et al, 2025, Outcomes of an Advanced Epic Personalization Course on Clinician Efficiency through Use of Electronic Medical Records: Retrospective Study, JMIR Formative Research, 9(), e68491, 10.2196/68491
