Entrance Surface Dose (ESD) Measurement During Pediatric Chest X-Rays
Abstract
Introduction
Given the high radiation tissue sensitivity of pediatric patients, it is necessary to monitor their received dose in order to optimize radiation protection. The first aim of this study was to evaluate of the entrance surface dose (ESD) in pediatric patients undergoing chest x-ray at the main hospital of Dezful, Iran. The second aim was to compare our results with the established dose reference levels (DRL).
Materials and Methods
The studied population included 204 pediatric patients less than 15 year who were referred to chest x-ray. A calibrated dose area product meter (DAP-meter) with permanent installation on x-ray unit was used to radiation dose measurements. For each patient, the demographic data, exposure parameters and the dose read by DAP-meter were recorded and ESD was calculated using standard mathematical formula.
Results
The average value of ESD was 119 μGy in patients less than 15 years. This value was 51.3, 122.3, 131.5 and 171.2 μGy for the age groups less than 1 year, 1 to 5 year, 5 to 10 year and 10 to 15 year, respectively. A statistical significant difference was seen between ESD values in different age groups (P<0.001), whereas no statistical difference was seen between ESD values in girls and boys (P =0.993).
Conclusion
Pediatric patients in hospital investigated (except age group less than 1 year) are subjected to unnecessary radiation exposure, especially due to use of non-optimize x-ray protocols.
Author Contributions
Academic Editor: Qiuqin Tang, Obstetrics and Gynecology Hospital Affiliated to Nanjing Medical University, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2020 Roya Davoodi, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Although discovery of X-rays by Wilhelm Conrad Rontgen in 1895 has revolutionized medical care, their use involves some potential health risks to an individual patients undergoing diagnostic and therapeutic procedures 1. This risk has established to be inversely proportion with patients age, suggests high radiation tissue sensitivity of pediatric patients. Several studies have reported that pediatrics to be as much as 10 times more susceptible to radiation induce carcinogenesis than adult 2, 3, 4. Therefore, it is necessary to monitor their received radiation dose, especially for frequent X-ray examinations in order to radiation protection optimization.
Chest X-ray is one of the frequent X-ray examinations requests by pediatricians for pediatric patients 4. Even though the radiation dose associated with a singular chest X-ray is low, but due to wide frequency, radiation dose optimization should be considered 4. Evidence showed that there is wide variation in the amount of radiation dose received by pediatric patients for the same type of X-ray examinations such as the chest X-rays 5, 6, 7. These variations result in some patients receives more radiation dose than needed. Accordingly, the international commission on radiological protection (ICRP) has recommended diagnostic reference levels (DRL) as a guide to protect patients from undue radiation exposure 8. DRL determine through the third quartile of the average entrance surface dose (ESD) distribution 9. ESD which is define as the absorbed dose at the entrance surface of the tissue, has been identified as the best indicator for monitor patients dose during X-ray examinations 10, 11. It can measure directly using thermoluminescent dosimeters (TLD) or indirectly by mathematical formula based on tube output at free-air or dose area product meter (DAP-meter) 10, 12, 13. There are rarely studies on radiation dose measurement during pediatric chest X-rays in Iran. Bahreyni Toossi et al. 5 reported ESD value of 76.3 µGy and DRL value of 88 µGy for neonatal chest X-rays in Mashhad. Similarly, Faghihi et al 14 reported ESD value of 56.6 µGy for neonatal chest X-rays in Shiraz.
The aim of this study was to evaluate of the ESD in pediatric patients undergoing chest X-ray using TLD and DAP-meter at large teaching hospital of Dezful-Iran.
Materials and Methods
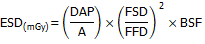
This study was performed during a period of 6-months in the radiology center of the teaching hospital of Dezful University of Medical Sciences (Dr. Ganjavian). Exposures were performed using a single digital radiography unit (VARIAN X-ray system, UAS) with total filtration of 3-mm aluminum and focal spot of 1-mm2. This unit has a fixed anti-scatter radiation grid that allows all exposure to be performed using the grid. Prior the study, approval was provided from the university ethic committee to proceed. Moreover, informed consent was obtained from the parents. The studied population included 204 pediatric patients who were referred to clinically indicated chest x-ray. Patients were considered eligible for inclusion if their age was less than 15 year, have anteroposterior (AP) or posteroanterior (PA) view of the chest x-ray on their request sheet and their parents has signed informed consent form. The emergency patients and patients with lateral view of the chest x-ray were excluded from the study. Following literatures 6, 12, 15, patients were divided into four age groups of less than 1 year, 1 to 5 year, 5 to 10 year and 10 to 15 year. For each patient, the demographic data and exposure parameters was measured and recorded. A calibrated dose area product meter (DAP-meter) with permanent installation on x-ray unit was used to radiation dose measurements. DAP is defined as the absorbed dose multiplied by the area of tissue irradiated which reflects dose in the radiation field together with area of tissue irradiated. ESD was calculated using the follow mathematical formula.
Where, A is the area of radiation field on the patient skin (cm2), DAP: dose measured by DAP-meter (mGy×cm2), FSD: x-ray focus to skin distance (m), FFD: x-ray focus to film distance (m) and BSF: back scatter factor.
Statistic
Data were entered into Microsoft Excel (Microsoft Inc., Redmond, WA) and statistical analysis was performed using SPSS software (IBM, Armonk, New York). The one-way analysis of variance (ANOVA) was used to measure and compare ESD values in different age groups. Moreover, independent paired t-test was used to compare ESD values in the boy and girl subjects.
Results
Of 204 pediatric patients enrolled in the study, 81 (39.7%) of whom were girl and 123 (60.3%) were boy. The characteristic of patients and exposure parameters are presented in Table 1. The average value of ESD was 119 μGy in patients less than 15 year. This value was 51.3, 122.3, 131.5 and 171.2 μGy for the age groups less than 1 year, 1 to 5 year, 5 to 10 year and 10 to 15 year, respectively (Figure 1). There was statistical significant difference between ESD value in different age groups (P<0.001). Increasing patients' age was resulted in increasing ESD value. There was significant correlation between applied current-time-product (mAs) and tube potential (kVp) with ESD values, whereas no meaningful correlation was found for patients sex (P=0.993).
Table 1. Characteristic of patients and exposure parameters during pediatric chest x-rays.| Variable | Average (range) | Standard deviation |
| Weight (kg) | 17.87 (2.50-50) | 11.8 |
| Height (cm) | 83.25(12-140) | 20.51 |
| A (cm2) | 24.71(18-30) | 4.73 |
| FFD (cm) | 118.87(35-150) | 24.29 |
| FSD (cm) | 104.2(18-123) | 18.4 |
| kVp | 67.59 (50-90) | 9.08 |
| mAs | 8.75(4-20) | 3.55 |
| DAP (mGy.cm2) | 33.94(4.8-87) | 19.86 |
Figure 1.Average ESD in pediatric patients undergoing chest x-ray as a function of patient age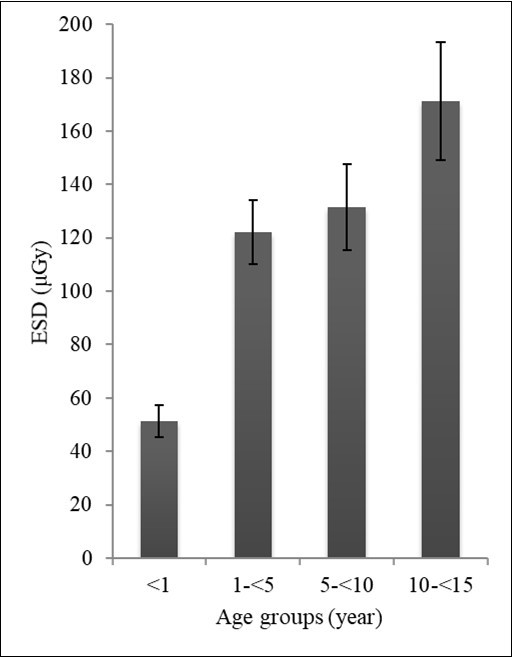
Discussion
Patient radiation dose measurement is crucial in order to optimize radiological protection in x-ray centers. This study provides useful information about the radiation dose received by pediatric patients undergoing chest x-ray at our hospital. It can be used for comparing patients' dose with the established DRL values so that patients do not receive unnecessary radiation exposure than needed. According to our results, the average ESD value for patients less than 1 year, 1 to 5 year, 5 to 10 year and 10 to 15 year were 51.3, 122.3, 131.5 and 171.2 μGy which are consistent with 66.14, 104.58, 135.77 and 139.03 μGy reported by Atalabi et al. for pediatric chest x-rays, respectively 6. The ESD value of 51.3 μGy measured in this study for the age group less than 1 year is consistent with 56.6 and 52 μGy reported by Faghihi et al 14 and Smans et al 16 for neonatal chest x-rays, whereas, it was lower than 76.3 μGy reported by Bahreyni Toossi et al 5. Both agreement and discordance was present between our study and the study performed by Ademola et al. 15 on pediatric chest x-rays. They reported ESD value of 111 and 159 μGy for the age group of 1 to 5 year and 5 to 10 year which are similar to 122.3 and 131.5 μGy obtained in our study. However, they reported ESD value of 620 μGy for 10 to 15 year patients which are substantially higher than 171.2 μGy obtained in our study. Similarly, our results are inconsistent with ESD value of 182, 172, 340 and 587 μGy reported by Zewdu et al for patients less than 1 year, 1 to 5 year, 5 to 10 year and 10 to 15 year during chest x-rays 12. These variations could be explained by variation in the applied FSD and exposure parameters (kVp and mAs), patient habitus, use or not use of anti-scatter grid and x-ray unites used in these studies. We found no significant correlation between patients' sex and weight with ESD values, whereas, significant correlation was seen for the applied kVp and mAs. These results are consistent with the literatures 6.
The DRL value of 50, 70 and 120 μGy has been recommended for a 1 year, 5 year and 10 year pediatric patient undergoing chest x-ray, respectively 7. Our results are consistent with the recommended DRL value of 50 μGy for age group less than 1 year. However, for age group 1 to 5 year and 5 to 10 year, the ESD value of 122.3 and 131.5 μGy measured in this study are higher than recommended DRL value of 70 and 120 μGy which refers to non-optimization of radiological protection for these age groups. Patient dose is particularly influence by variation in the applied exposure parameters 12. The European Commission (EC) has recommended tube potential (kVp) of 60 to 80 for pediatric patients less than 1 year and 100 to 120 for 5 year and higher 17. The use of tube potential less than 60 kVp has also been discouraged. This advice comes from this fact that appropriate combining use of high kVp and low mAs would result in reducing patient dose 5. In this study, the radiographers were used of 60 to 65 kVp for patients less than 1 year, 63 to 70 for 1 to 5 year, 65 to 70 for 5 to 10 year and 65 to 75 kVp for 10 to 15 year patients. These inappropriate exposure parameters clearly indicate that the protocols used for pediatric chest x-rays (except for age group less than 1 year) are not optimized. Such concern has been reported in the literatures 12, 15.
Conclusion
This study indicated that 1 to 15 year pediatric patients in hospital investigated are subjected to unnecessary radiation exposure, especially due to use of non-optimize x-ray protocols. We recommend provision and adherence to a written departmental radiation safety protocol in order to protect pediatric patients from undue exposure to radiation.
Acknowledgements
This study was extracted from the MSc thesis of the first author and a research project approved by Payam-Noor University of Mashhad.
References
- 1.Ward R, Carroll W D, Cunningham P, Ho S-A, Jones M et al. (2017) Radiation dose from common radiological investigations and cumulative exposure in children with cystic fibrosis: an observational study from a single UK centre. , BMJ open 7(8), 17548.
- 2.Curtis J R. (2010) Computed tomography shielding methods: a literature review. Radiologic technology. 81(5), 428-36.
- 3.Hohl C, Wildberger J, Süß C, Thomas C, Mühlenbruch G et al. (2006) Radiation dose reduction to breast and thyroid during MDCT: effectiveness of an in-plane bismuth shield. , Acta Radiologica 47(6), 562-567.
- 4.Kostova-Lefterova D, Taseva D, Hristova-Popova J, Vassileva J. (2015) Optimisation of paediatric chest radiography. Radiation protection dosimetry.165(1-4):. 231-4.
- 5.MTB Toossi, Malekzadeh M. (2012) Radiation dose to newborns in neonatal intensive care units. , Iranian Journal of 9(3), 145.
- 6.Atalabi O M, BidemiI A, Adekanmi A J, Samuel O A. (2013) Entrance surface dose from pediatric diagnostic x-ray examinations in a developing world setting: are we'ALARA principle'compliant?. , British Journal of Medicine and Medical 3(4), 2288.
- 7.Kim B H, Do K-H, Goo H W, Yang D H, Oh S Y et al. (2012) National survey of radiation doses of pediatric chest radiography in Korea: analysis of the factors affecting radiation doses. Korean journal of radiology. 13(5), 610-7.
- 8.Nikupaavo U, Kaasalainen T, Reijonen V, Ahonen S-M, Kortesniemi M. (2015) Lens dose in routine head CT: comparison of different optimization methods with anthropomorphic phantoms. , American Journal of Roentgenology 204(1), 117-23.
- 9.Freitas M B, Yoshimura E M. (2009) Diagnostic reference levels for the most frequent radiological examinations carried out in Brazil. Revista Panamericana de Salud Pública. 25, 95-104.
- 10.Jornet N, Muñoz J, Martin-Viera J, Jurado D, Pallerol R et al.. , DETERMINATION OF ENTRANCE SURFACE DOSE IN STANDARD EXPLORATIONS IN RADIODIAGNOSTIC
- 11.Ofori K, Gordon S W, Akrobortu E, Ampene A A, Darko E O. (2014) Estimation of adult patient doses for selected X-ray diagnostic examinations. , Journal of Radiation Research and Applied Sciences 7(4), 459-62.
- 12.Zewdu M, Kadir E, Berhane M. (2017) Assessment of pediatrics radiation dose from routine x-ray examination at Jimma University Hospital, Southwest Ethiopia. Ethiopian journal of health sciences. 27(5), 481-90.
- 13.Gholami M, Maziar A, Khosravi H, Ebrahimzadeh F, Mayahi S. (2015) Diagnostic reference levels (DRLs) for routine X-ray examinations in Lorestan province. , Iran. International Journal Of Radiation Research 13(1), 85.
- 14.Faghihi R, Mehdizadeh S, Sina S, Alizadeh F N, Zeinali B et al. (2011) Radiation dose to neonates undergoing X-ray imaging in special care baby units in Iran. Radiation protection dosimetry. 150(1), 55-9.
- 15.Ademola A, Obed R, Adejumobi C, Abodunrin O, Alabi O et al. (2013) Assessment of Entrance Skin Dose in routine x-ray examinations of chest, skull, abdomen and pelvis of children in five selected hospitals in Nigeria. , IOSR Journal of Applied Physics 5(2), 47-50.
Cited by (2)
This article has been cited by 2 scholarly works according to:
Citing Articles:
Calabar Journal of Health Sciences (2022) Crossref
G. Inah, E. Ukpong, E. Esien-umo, B. Ibe, A. Ijever et al. - Calabar Journal of Health Sciences (2022) Semantic Scholar
Calabar Journal of Health Sciences (2022) OpenAlex