Spontaneous Subgaleal Hemorrhage in a Child with Autism
Abstract
Severe ascorbic acid (Vitamin C) deficiency, commonly known as “scurvy,” continues to be a problem in malnourished populations across the world but is relatively rare in the United States. Early features of this condition include general weakness, fatigue, and aching limbs. An extremely rare and late feature of this condition is subgaleal hemorrhage. Scurvy has such a low prevalence in First World countries that it is often misdiagnosed or not diagnosed at all. The subject in this case report presented acutely and is one of few to involve a subgaleal hemorrhage to be documented in medical literature to date. Laboratory studies and clinical improvement through treatment established the diagnosis. Ascorbic acid deficiency should be considered when evaluating children with poor nutrition despite socioeconomic status, living conditions, or access to health care. This case also reminds us that neurodivergent children are a vulnerable population and more research will need to be conducted to determine just how detrimental the pandemic has been to patients with ongoing problems who were lost to follow up.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2023 Jennifer W. Glusman, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Author note
Co-author credentials: Jennifer W. Glusman (DO, MAT); Anne K. Doran (MD).
Competing interests
The authors have declared that no competing interests exist.
Citation:
Background
In developed nations, scurvy is an incredibly rare condition due to the availability of nutrient rich foods to most inhabitants. In the United States, only about 7% of the population is estimated to have a Vitamin C deficiency.1 Vitamin C deficiency does not necessarily equate to the development of scurvy, however. Symptoms of scurvy typically only present when plasma Vitamin C concentrations reach a level of 0.2 mg/dL.2 Although bone pain is a classic presentation of scurvy, if the patient presents early enough, imaging such as skeletal surveys and MRIs can be normal (Figure 2B - 2I) which often leads practitioners astray.3 Generally, scurvy is observed in populations of lower socioeconomic status, the elderly, and alcoholics.4 Given the low rates of scurvy across the United States and the fact that our patient did not belong to any classic high-risk groups, this case is particularly unusual.
This condition is uncommon, and the development of subsequent subgaleal hemorrhage is even more rare. There is little documentation of subgaleal hemorrhage associated with scurvy.5Further research and publication demonstrating the connection between these two processes may help physicians in making an earlier diagnosis of scurvy in future cases.
Case Report
This patient is a four-year-old male with a primary medical history of non-verbal autism who presented to the emergency department in March 2022 with rash for two months, non-ambulatory status for two weeks, poor oral intake for six days, and dental pain.
Two months prior, he had a COVID-19 infection which resulted in mild congestion, fevers and an erythematous rash on his cheeks that spread to his arms and legs. One month later, he was brought to his pediatrician for leg pain. His pediatrician diagnosed him with transient synovitis secondary to his COVID-19 infection and recommended ibuprofen until his pain subsided. One month later, this patient went to urgent care for worsening leg pain despite taking ibuprofen as instructed. X-rays of his bilateral hips and pelvis were negative. Two weeks later, he stopped ambulating and was brought to the emergency department. His mother noted a pruritic rash on his legs, decreased oral intake, and felt like her son was in pain. Lab work revealed normal coagulation factors, electrolytes, albumin, ESR, CRP, and urinalysis. WBC count, hematocrit, and absolute lymphocyte count were all low at 5.9 K/mcL, 33%, and 2.8 K/mcL. Repeat X-rays of his left femur and ultrasound of bilateral hips were unremarkable. The patient was instructed to take Naproxen twice daily and to see orthopedics outpatient in two weeks. The patient continued to take his ibuprofen instead of the recommended Naproxen. He was seen at outpatient orthopedics two weeks later, where his persistent non-ambulatory status prompted a referral back to the emergency department.
At this time, the mother endorsed a new boggy swelling on the top of his head that started earlier that morning, but denied any history of trauma. She noted swelling and erythema on his upper left maxilla where he was missing a tooth. In the past six days, he had tolerated fluids but had poor solid food intake and worsening fatigue. On exam, the patient was thin-appearing, lethargic, and febrile to 38 degrees Celsius with otherwise normal vital signs. His hips were externally rotated in bed, with no obvious deformity or edema. Passive range of motion of bilateral hips, knees, and ankles were all without pain, joints were non-tender without swelling. He had equal strength of all extremities while laying down but refused to ambulate. He had folliculitis on his upper extremities, and petechiae on his bilateral lower and upper extremities, cheeks, and back with sparing of the chest and trunk. He had diffuse bogginess noted over his right parietal and temporal skull, a draining dental abscess surrounding his erupting first molar on the left upper maxilla, and abdominal tenderness in the right upper quadrant. Lab work revealed thrombocytopenia of 79 K/mcL, hemoglobin of 10.4 g/dL, hypokalemia of 3.1 mmol/L, elevated lactate dehydrogenase of 325 Units/L, with normal acute phase reactants, hepatic liver enzymes, creatine, creatine kinase, and uric acid. Upon further questioning, the patient’s mother endorsed that he is an extremely picky eater and only eats macaroni and cheese and pancakes. Furthermore, he has never consumed a fruit or vegetable in his lifetime, and he lost his speech therapy services during the pandemic.
The differential at that time was broad. There are case reports of post-COVID-19 immune mediated thrombocytopenia and ITP, but this did not explain this patient’s entire clinical picture. His compromised nutritional status made him high-risk for vitamin deficiencies, but obtaining vitamin levels would take several days. The patient’s dental abscess could be due to poor baseline dentition as the patient had never seen a dentist, and the patient’s mother found it difficult to brush his teeth. It was unclear if his impaired mobility was secondary to abdominal pain, malnutrition, an acute infectious process such as osteomyelitis, or all of the above. The boggy area on his skull was concerning for a hematoma; there were no intracranial findings on CT and seemingly no history of trauma, however, his thrombocytopenic state made him more at risk for injury. This patient’s severe autism also made him high-risk for non-accidental trauma.
From a musculoskeletal standpoint, MRIs of the cervical, thoracic, and lumbar spine were within normal limits. The patient was started on scheduled acetaminophen for pain management. A CT of the head without contrast showed right high convexity scalp soft tissue swelling without acute intracranial abnormality (Figure 1A – 1F). A complete bone survey was negative for sources of trauma (Figure 2B – 2I) but did note calvarial soft tissue edema (Figure 2A). A head ultrasound confirmed the fluctuance on the patient’s skull to be a subgaleal hemorrhage (Figure 3A – 3C) of 9 mm thickness at its greatest.
Figure 1A - 1F.Noncontrast CT examination of the brain. Multiple axial images were obtained. Images listed from superior to inferior. Adjustment of the MA and/or KV was done according to the patient's size. Findings include right high convexity scalp soft tissue swelling without acute intracranial abnormality.
Figure 2A - 2J.X-Ray complete bone survey. 2A: Lateral view of the skull, 2V. 2B: Frontal view of chest, abdomen and pelvis (spine), 1V. 2C: Frontal view of left humerus, 2V. 2D: Frontal view of left hand, 2V. 2E: Frontal view of right humerus, 2V. 2F: Frontal view of right hand, 2V. 2G: Frontal view of both femora, 1V. 2H: Frontal views of both lower legs, 2V. 2I: Frontal views of both feet, 2V. Findings include calvarial soft tissue edema. No additional injury detected on these radiographs.
Figure 3A – 3C.Ultrasound soft tissue head using multiplanar gray scale and color Doppler images. The superficial subcutaneous soft tissue appears homogeneous and uniform thickness. There is a layer of heterogeneous echogenicity deep to the subcutaneous layer, on the surface of the bone which appears retained by an echogenic capsule or membrane. This measures up to 9 mm greatest thickness. The size of the collection is greater than the transducer can measure. Additional images performed to include the edges of the hemorrhage show uplifting of the galea consistent with subgaleal location. The cranial sutures are not adequately included.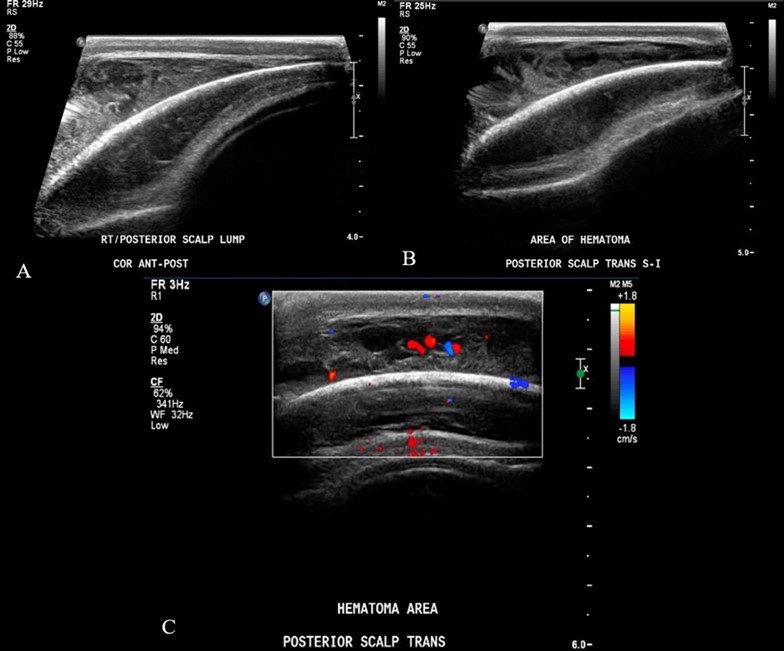
From an infectious disease point of view, the patient’s EBV Capsid Antibody IgM was found to be elevated, but the rest of his infectious workup was negative aside from his dental abscess, which was treated with intravenous ampicillin-sulbactam. The patient remained afebrile for the rest of his hospital stay. From a nutrition standpoint, Vitamin A, D, E, K, C, zinc, B12, folate, thiamine, iron studies, and MMA levels were all sent. Vitamin B12 was very elevated (>2000 pg/ml, normal range 211 – 911), Vitamin D was low (23.7 ng/mL, normal range 30 – 100), and Zinc was low (64 mcg/dL, normal range 70 – 120). The patient was started on Vitamin D and Zinc supplementation, and IV Omeprazole 0.5 mg/kg twice daily for presumed NSAID-induced gastritis. The medical team had a high suspicion of ascorbic acid deficiency based on his history, and so was started on high dose IV Vitamin C infusions shortly after admission. Seven days after the patient was admitted, his Vitamin C level resulted at an extremely low level (<5 umol/L, normal range 23 - 114), at which point he was officially diagnosed with scurvy. All other vitamin levels and iron studies were within normal limits. Hematologically speaking, the thrombocytopenia resolved without other interventions. His hemoglobin continued to downtrend while inpatient, but he remained hemodynamically stable and his subgaleal hemorrhage did not increase in size during his hospital stay. The patient worked extensively with physical therapy and occupational therapy during his nine-day hospital stay.
On discharge, the patient was able to walk across his room and short distances down the hallway, no longer required acetaminophen, and was eating and drinking by mouth. The patient’s folliculitis and petechia improved, and his subgaleal hemorrhage decreased in size substantially. His abdominal pain, dental abscess, and anemia resolved. The patient was discharged on Vitamin D, C (125 mg daily), Zinc, and multivitamin supplementation with close follow up.
Discussion and Conclusions
The mother of our patient has two children with severe non-verbal autism, which makes this case even more concerning; her children see physicians more often than children who are not neurodivergent, giving them more opportunities to be monitored closely for nutrition than most children. Many parents of children with autism spectrum disorder face challenges in providing a balanced diet for their children. Unfortunately, nutrition is often forgotten about for said patients as other medical concerns frequently take priority in a short office visit. The authors of this case report hope that this case reminds providers to discuss nutrition with parents of neurodivergent children early and often to gauge whether dietary requirements are being met.
What cannot be ignored is how much more at risk neurodivergent children were during the pandemic due to a national shortage of medical services. With no access to speech therapy for several years, this patient was lost to follow up and greatly suffered the consequences. There is very little literature on how detrimental the pandemic was to patients with ongoing medical problems. More research needs to be conducted to determine how far behind these children are in developmental milestones and nutrition, and what interventions will be needed to catch them up.
Ultimately, encouraging open and honest communication between providers and parents will help to prevent severe nutritional deficiencies and the devastating consequences they can have, as seen in this case report. Broaching the topic of nutrition with a caring and judgement-free approach will encourage more honesty between parents and providers and lead to better outcomes for neurodivergent children everywhere.
References
- 1.Schleicher R L, Carroll M D, Ford E S, Lacher D A. (2009) Serum vitamin C and the prevalence of vitamin C deficiency in the United States: 2003–2004 National Health and Nutrition Examination Survey (NHANES),The. , American Journal of Clinical 90(5), 1252-1263.
- 2. (2000) National Academies Press.Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium and Carotenoids. Washington DC:.
