Validity of PIRO Score as an Assessment Tool for Mortality Risk of COVID-19 Pneumonia among Patients Admitted to World Citi Medical Center from March to August 2020. A Retrospective Observational Cohort Study
Abstract
Introduction
In December 2019, cases of serious illness causing pneumonia and death were first reported in Wuhan, China.2 The clinical features of Corona Virus Disease-19 (COVID-19) are ranging from asymptomatic to multi organ dysfunction. The disease can progress to pneumonia, respiratory failure and death.4 Thus, a tool is needed that can predict the severity and in-hospital mortality risk of a patient with COVID-19 Pneumonia.
The PIRO (predisposition, insult, response, and organ dysfunction) scoring was developed for use in the emergency department to risk stratify sepsis cases.15 Eventually it was adapted in pneumonia cases to predict its severity.
Objective
To validate PIRO score as an assessment tool for COVID-19 mortality risk among patients with confirmed COVID-19 RT-PCR test among patients aged 19 and above admitted in World Citi Medical Center from March 2020 to August 2020
Methods
This study included 93 patients aged 19 and above admitted in World Citi Medical Center with a primary diagnosis of COVID-19 Confirmed with pneumonia between March 2020 to August 2020. The patients’ charts were retrieved from the hospital medical records and case notes were reviewed. A severity assessment score was developed based on PIRO score (Predisposition comorbidities and age; Insult multilobar opacities and viremia; Response shock and hypoxemia; Organ Dysfunciton) were extracted. The patients were stratified in four levels of risk: a)Low,0-2 points; b)Mild,3 points; c)High,4 points; d)Very High,5-8 points. The PIRO score and the clinical outcome were compared. The discriminative ability of PIRO score to predict mortality risk was evaluated under receiver operating characteristic curve (AUC).
Results
The PIRO score had an excellent predictive ability for in-hospital mortality (AUC0.9197). Analysis of variance showed that higher levels of PIRO scores were significantly associated with higher mortality (p<0.001). Patients with Mild PIRO risk category were 98.65% less likely to expire (p<0.001, 95%CI 0.0015) and High PIRO risk category were 94.47% less likely to expire (p<0.001, 95%CI 0.0124), both compared to patients with Very high PIRO risk category. Finally, Very High PIRO risk category were more than 44 times likely to expire compared to patients with Low, Mild and High PIRO risk category (p<0.001, 95%CI 11.738).
Conclusions
The PIRO score is a valid risk model that can be used to predict in-hospital mortality, that can help clinicians provide timely and accurate assessment, and hence appropriate management to patients with COVID-19 Pneumonia.
Author Contributions
Academic Editor: Raul Isea, Fundación Instituto de Estudios Avanzados - IDEA, Hoyo de la Puerta, Baruta.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2021 Graciano D. Natividad III, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Background
In December 2019, cases of serious illness causing pneumonia and death were first reported in Wuhan, the capital of Hubei, China. Soon after, the number of cases soared dramatically, spreading across China and worldwide 2 On January 9, 2020, the Chinese Center for Disease Control and Prevention (Chinese CDC) declared the identification of a novel Coronavirus 1 A few days later, it was reported that this novel type of coronavirus, termed by the WHO as novel coronavirus-2019, Severe acute respiratory syndrome coronavirus 2 (SARSCoV- 2), was responsible for the outbreak 2 All ages are susceptible. Infection is transmitted through large droplets generated during coughing and sneezing by symptomatic patients but can also occur from asymptomatic people and before onset of symptoms 4
The clinical features of Corona Virus Disease 2019 (COVID-19) are varied, ranging from asymptomatic state to acute respiratory distress syndrome and multi organ dysfunction. The common clinical features include fever (not in all), cough, sore throat, headache, fatigue, headache, myalgia and breathlessness. Thus, they are indistinguishable from other respiratory infections. In a subset of patients, by the end of the first week, the disease can progress to pneumonia, respiratory failure and death. 4 On January 30, 2020 the Philippines reported its first two imported cases of COVID-19 in a couple from Wuhan. One of them died on February 1st, 2020 becoming the first COVID-19 death outside China 5, 6, 7. As of November 21, 2020 there are 415, 067 total cases; 375, 237 are recovered cases with a total of 8,025 death cases. 17Thus, we need a tool that can be easily used to predict the severity and in-hospital mortality risk of a patient with COVID-19 Pneumonia.
Originally, PIRO (predisposition, insult, response, and organ dysfunction) scoring was developed for use in the emergency department (ED) to risk stratify sepsis cases, 15 but in 2003, an international panel of experts participated in a consensus conference sponsored by Society of Critical Care Medicine, European Society of Intensive Care Medicine, American College of Chest Physicians, ATS, and Surgical Infection Society which introduced PIRO as a hypothesis-generating model for future research. Eventually, in 2009, PIRO scoring system was used in pneumonia cases to predict its severity. The elements of the PIRO concept are: Predisposition (chronic illness, age, and comorbidities); Insult (injury, viremia); Response (hypoxemia, hypotension); and Organ dysfunction. 8, 9
Significance of the Study
COVID-19 pneumonia does not have any objective measurement or tool to help identify its mortality risk.
To be clinically useful, the assessment tool or risk model should be simple, readily measurable, easily accessible, reliable, non-invasive and most of all in expensive. This study aims to provide an objective measure in determining the in-hospital mortality risk of COVID-19 Pneumonia in adult patients, aged 19 and above, with confirmed diagnosis of COVID-19 Pneumonia using the PIRO score.
Objectives
General Objective
The purpose of this study is to validate PIRO score as an assessment tool for COVID-19 mortality risk among patients with confirmed COVID-19 Reverse Transcriptase – Polymerase Chain Reaction (RT-PCR) test among patients aged 19 and above admitted in World Citi Medical Center from March 2020 to August 2020.
Specific Objectives
To determine the PIRO score of admitted patients, aged 19 and above, with pneumonia and COVID-19 Confirmed RT PCR test
To correlate the PIRO score of admitted patients, aged 19 and above, with pneumonia and COVID-19 Confirmed RT PCR test with the clinical outcome
Methodology
Study Design
This is a retrospective observational cohort study of adult patients, aged 19 and above, admitted at World Citi Medical Center with a primary diagnosis of Coronavirus Disease-19 Pneumonia between March 01, 2020 to August 31, 2020.
Study Settings
The study was performed in World Citi Medical Center, an adult urban tertiary hospital with 150 bed capacity. The Emergency Department (ED) has approximately 12,000 non-trauma patients per year, and 20% seek medical care for respiratory symptoms.
Study Subjects
All the consecutive adult patients (age 19 and above) admitted to hospital through the ER with a final diagnosis of COVID-19 Pneumonia (International Classification of Diseases, 10th revision, Clinical Modification, ICD-10 CM code UO7) Confirmed by RT-PCR and chest radiograph or high resolution chest CT-scan, between 01 March–31 August 2020 were included.
Data Collection
The patients’ charts were retrieved from the hospital medical records and case notes were reviewed by the investigators. The variables required for PIRO score (predisposition, insult, response, and organ dysfunction) including the presence of the following: comorbidities (COPD, immunocompromise); age >70 years; multilobar opacities in chest radiograph or chest CT-scan; shock, severe hypoxemia; acute renal failure; viremia and acute respiratory distress syndrome were extracted. The patients were stratified in four levels of risk: a) Low, 0-2 points; b) Mild, 3 points; c) High, 4 points; d) Very High, 5-8 points. The PIRO score and the clinical outcome was compared. The discriminative ability of PIRO score to predict mortality risk was evaluated under receiver operating characteristic curve (AUC).
COVID-19 Confirmed Pneumonia Definition
In this study, COVID-19 Confirmed Pneumonia were cases with RT-PCR result of positive for RNA Corona Virus Disease 19 with evidence of Pneumonia either via chest radiograph or chest CT-scan.
Inclusion Criteria
Patients were aged 19 and above, who were admitted in World Citi Medical Center from March 01, 2020-August 31, 2020, with RT-PCR confirmed COVID-19 and pneumonia via chest radiograph or chest CT scan.
Exclusion Criteria
Patients with confirmed COVID-19 RT-PCR test but with no evidence of pneumonia either via chest radiograph or chest CT-scan, aged 18 years and 364 days and younger and patients admitted outside the inclusion dates of March 2020 to August 2020 were all excluded.
Severity Score Calculation and Stratification
The PIRO score was obtained from the data extracted from patients’ charts. One point was given for each present feature (range, 0-8 points). Patients were subsequently stratified into different levels of risk groups: (a) Low risk (0-2 points); (b) Mild risk (3 points); (c) High risk (4 points); (d) Very high risk (5-8 points); The primary outcome of in-hospital mortality were compared.
Sample Size 14
A minimum of 41 patients were required for this study based on 0.88 AUC of PIRO score to predict 28-day mortality among patients with community-acquired pneumonia10, 5% level of significance and 10% desired half-width of the confidence interval.
Statistical Analysis
Descriptive statistics was used to summarize the demographic and clinical characteristics of the patients. Frequency and proportion was used for categorical variables, median and inter quartile range for non-normally distributed continuous variables, and mean and SD for normally distributed continuous variables. Independent Sample t-test, Mann-Whitney U test and Fisher’s Exact/Chi-square test was used to determine the difference of mean, rank and frequency, respectively, between recovered and expired patients. Odds ratio and corresponding 95% confidence intervals from binary logistic regression was computed to determine significant predictors for in-hospital mortality. Sensitivity, Specificity, NPV, PPV, and Area under the Receiver operating characteristics curve were used to determine the diagnostic accuracy of PIRO score to predict in-hospital mortality. All statistical tests were two tailed test. Shapiro-Wilk was used to test the normality of the continuous variables. Missing variables wereneither replaced nor estimated. Null hypotheses were rejected at α = 0.05 level of significance. STATA 13.1 was used for data analysis.
Methods of Data Collection
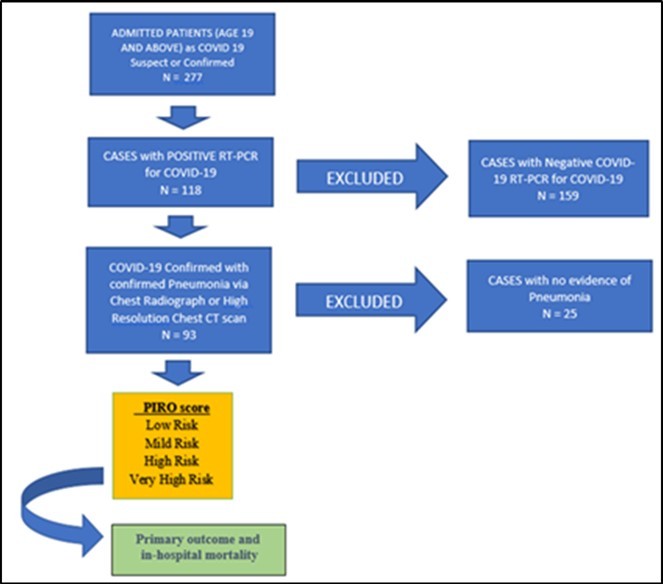
There were 277 subjects admitted as either COVID-19 Suspect or Confirmed. 159 subjects were excluded for testing negative for COVID-19 RT-PCR and 25 subjects were excluded for having no evidence of pneumonia either by chest radiograph or chest CT-scan. A total of 93 patients met the inclusion criteria.
Results
This study included 93 patients with a primary discharged diagnosis of COVID-19 pneumonia at World Citi Medical Center from March 01, 2020 to August 31, 2020. Table1 shows the demographic profile of the patients. There were 93 patients with a confirmed diagnosis of COVID-19 Pneumonia, mild to critical. Among these 93 patients, 24 (26%) of which expired and 69 (74%) were recovered and discharged. There was statistical difference between recovered and expired patients in terms of Age (p<0.001), Hypertension (p<0.049), COPD (p<0.022), PIRO score (p<0.001) and PIRO category (p<0.001). Figure 1
Figure 1.PIRO score had a calculated AUC of 0.9197 for predicting in-hospital mortality for COVID-19 Pneumonia indicating that it has an excellent discriminative ability.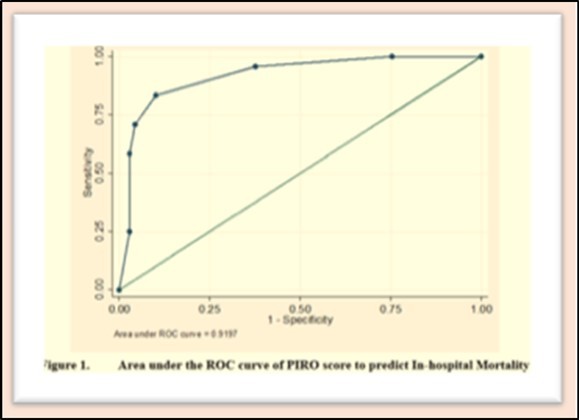
| Total (n=93) | Expired (n=24, 26%) | Recovered (n=69, 74%) | P-value | |
| Frequency (%); Mean + SD; Median (IQR) | ||||
| Age | 56.7 ± 18.08 | 67.42 ± 18.12 | 52.97 ± 16.63 | <0.001 |
| Sex | 0.634 | |||
| Male | 53 (56.99) | 15 (62.5) | 38 (55.07) | |
| Female | 40 (43.01) | 9 (37.5) | 31 (44.93) | |
| Comorbidities | ||||
| Hypertension | 46 (49.46) | 16 (66.67) | 30 (43.48) | 0.049 |
| Diabetes Mellitus | 27 (29.03) | 9 (37.5) | 18 (26.09) | 0.289 |
| COPD | 4 (4.30) | 3 (12.5) | 1 (1.45) | 0.022 |
| Cardiovascular | 20 (21.51) | 8 (33.33) | 12 (17.39) | 0.147 |
| Cerebrovascular | 1 (1.08) | 0 | 1 (1.45) | 1.000 |
| CA | 3 (3.23) | 2 (8.33) | 1 (1.45) | 0.162 |
| BA | 9 (9.68) | 3 (12.5) | 6 (8.7) | 0.690 |
| PTB | 4 (4.30) | 1 (4.17) | 3 (4.35) | 1.000 |
| Immunodeficiency | 1 (1.08) | 1 (4.17) | 0 | 0.258 |
| Chronic Kidney Disease | 12 (12.9) | 4 (16.67) | 8 (11.59) | 0.499 |
| Liver Pathology | 1 (1.08) | 0 | 1 (1.45) | 1.000 |
| PIRO score | 4 (3 to 5) | 7 (5 to 8) | 3 (3 to 4) | <0.001 |
| Low | 17 (18.28) | 0 | 17 (24.64) | <0.001 |
| Mild | 27 (29.03) | 1 (4.17) | 26 (37.68) | |
| High | 22 (23.66) | 3 (12.5) | 19 (27.54) | |
| Very high | 27 (29.03) | 20 (83.33) | 7 (10.14) | |
The mean age of patients with confirmed COVID-19 pneumonia was 56 years old. There was statistical difference between the mean age of those who expired was 67 and mean age of recovered was 52. In terms of gender, there were more males (56.99%) than females (43.01%) who got infected with COVID-19. Among the co-morbidities in patients with COVID-19 Pneumonia, Hypertension (49.46%) and Diabetes mellitus (29.03%) are the two most common. The two most statistically significant comorbidities that may have contributed to mortality risk are hypertension and COPD with P-value of 0.049 and 0.022, respectively.
Table 2shows the validity of PIRO score to predict in-hospital mortality. Analysis of variance showed that higher levels of PIRO score were significantly associated with higher mortality (p<0.001). Patients with Mild PIRO risk category were 98.65% less likely to expire compared to patients with Very high PIRO risk category (p<0.001, 95% CI (0.0015 – 0.1185)). Patients with High PIRO risk category were 94.47% less likely to expire compared to patients with Very high PIRO risk category (p<0.001, 95% CI (0.0124 – 0.2455)). Patients with Very High PIRO risk category were 44 times more likely to expire compared to patients with Low, Mild and High PIRO risk scoring category (p<0.001, 95% CI (11.738 – 167.09)). There was no mortality recorded among patients in the LOW risk category, and hence cannot be compared.
Table 2. PIRO score to predict in-hospital mortality| PIRO Scoring | Crude Odds ratio | 95% CI | P-value |
|---|---|---|---|
| Low riska | |||
| Mild riska | 0.0135 | 0.0015 to 0.1185 | <0.001 |
| High riska | 0.0553 | 0.0124 to 0.2455 | <0.001 |
| Very high riskb, | 44.2857 | 11.738 to 167.09 | <0.001 |
Table 3shows the sensitivity and specificity of PIRO to predict in-hospital mortality; sensitivity for PIRO score >5 to predict mortality is 83.33%, while specificity for PIRO score <5 to predict that the patient is less likely to expire is 89.86%.
Table 3. Diagnostic parameters of PIRO score to predict In-hospital Mortality| Expired | Recovered | ||
| Frequency (%) | Total | ||
| PIRO Score > 5 | 20 (83.33) | 7(10.14) | 27 (29.03) |
| PIRO Score <5 | 4 (16.67) | 62 (89.86) | 66 (70.97) |
| Total | 24 (100) | 69 (100) | 93 (100) |
| Sensitivity | 83.33%(62.62 to 95.26) | Positive LR | 8.21 (3.98 to 16.95) |
| Specificity | 89.86%(80.21 to 95.82) | Negative LR | 0.19 (0.08 to 0.46) |
| PPV | 74.07%(58.06 to 85.50) | Prevalence | 25.81% (17.29 to 35.92) |
| NPV | 93.94%(86.33 to 97.44) | Accuracy | 88.17% (79.82 to 93.95) |
Discussion
COVID-19 Pneumonia is caused by novel Coronavirus. The clinical features of COVID-19 are varied, ranging from asymptomatic state to acute respiratory distress syndrome and multi organ dysfunction. They are indistinguishable from other respiratory infections. In a subset of patients, by the end of the first week the disease can progress to pneumonia, respiratory failure and death. 4 Originally, PIRO scoring was developed for use in the emergency department (ED) to risk stratify sepsis cases. Eventually PIRO scoring system was used in pneumonia cases to predict its severity. 15
To our knowledge, this is the first study to objectively measure the mortality risk of COVID-19 pneumonia on the basis of risk category of PIRO scoring. Many other models have been developed, some of which are designed to predict mortality. The diversity of scoring tools may pose difficulties for clinicians who are attempting to choose a tool for use in their daily practice. 12 For a tool to be clinically useful, the assessment tool or risk models should be simple, readily measurable, easily accessible, reliable, non-invasive and most of all inexpensive. The simplicity of PIRO score makes it more practical to be used as it is based on four easily assessable components. 10 The validation of PIRO score as an assessment tool for COVID-19 mortality risk among patients with confirmed COVID-19 RT-PCR test aged 19 and above may assist clinicians in managing patients to give proper management in a timely manner.
There were 277 subjects admitted as either COVID-19 Suspect or Confirmed. 159 subjects were excluded for testing negative for COVID-19 RT-PCR and 25 subjects were excluded for having no evidence of pneumonia either by chest radiograph or chest CT-scan. A total of 93 patients met the inclusion criteria and among these patients, 24 (26%) of which expired and 69 (74%) were recovered and discharged. There was statistical difference between recovered and expired patients in terms of Age, Hypertension, COPD, PIRO score and PIRO category.
The mean age of subjects infected was 56.7 and mean age of subjects who expired is 67. Analysis showed that the older the age were significantly associated with higher mortality (p<0.001). Likewise in the study of Farha et al (September 2020), a significant association were found between mortality among COVID-19 infected patients and older age (>65 years vs <65 years) (RR 3.59, 95% CI (1.87-6.90), p<0.001). 18
The two most statistically significant comorbidities that may have contributed to mortality risk are hypertension and COPD with P-value of 0.049 and 0.022, respectively. It is parallel with the recent study of Farha et al (September 2020) shows that a significant association were found between mortality among COVID-19 infected patients and hypertension (RR 2.08, 95% CI (1.79-2.43), p<0.001). 18 Further, the study of Kunzmann (October 2020) showed that COPD has three-fold greater risk of mortality in Severe COVID-19 patients (OR 3.23; 95% CI (1.59-6.57), p <0.05). 19 Stabilizing these comorbidities may alter the clinical outcome of COVID-19 pneumonia, but these claim needs further study.
This tool can be used as an initial risk assessment and stratification that predicts not only the severity of COVID-19 Pneumonia but also in-hospital mortality. As observed in this study’s results, subjects with a PIRO score of 5 or more were 27 (29.03%) and 20 (83.33%) of these subjects expired; In contrast, the subjects with a PIRO score of less than 5 were 66 (70.97%) and 62 (89.96%) recovered. Patients with Mild PIRO risk category were 98.65% less likely to expire compared to patients with Very high PIRO risk category (p<0.001, 95% CI (0.0015 – 0.1185)). Patients with High PIRO risk category were 94.47% less likely to expire compared to patients with Very high PIRO risk category (p<0.001, 95% CI (0.0124 – 0.2455)). Patients with Very High PIRO risk category were 44 times more likely to expire compared to patients with Low, Mild and High PIRO risk scoring category (p<0.001, 95% CI (11.738 – 167.09)). There was no mortality recorded among patients in the LOW risk category, and hence cannot be compared.
These results showed that higher levels of PIRO score were significantly associated with higher mortality. (p<0.001) Further, the calculated AUC for predicting in-hospital mortality of COVID-19 Pneumonia is 0.9197, which shows that the tool has excellent discriminative ability. These findings were also parallel with the recent studies, by Pinera et al (2016), 13 which shows that PIRO score had a high discriminatory performance in ICU mortality with an AUC=0.878, as well as that of Esguerra-Llabado et al (2019) 12, which also showed an excellent discriminatory performance in in-hospital mortality with an AUC=0.9313.
Conclusion
The PIRO score can be used as an assessment tool to identify the severity and in-hospital mortality risk of COVID-19 pneumonia among patients, aged 19 and above. It is simple, readily measurable, easily accessible, reliable, non-invasive and most of all inexpensive.
Recommendations
A larger retrospective cohort study may be done in the future to assess the predictive capacity of PIRO for COVID-19 Pneumonia. A prospective cohort study could also be done to observe the subjects while admitted and to identify other possible factors affecting the clinical outcome. Lastly, we would like to recommend using PIRO score in a prospective study with COVID-19 pneumonia to possibly lower its mortality by aggressively managing affected systems before its failure and stabilizing comorbidities such as hypertension and COPD that may alter the clinical outcome.
Limitations
Our study was limited by being a retrospective and single-center study. This study also had a relatively small sample size with limited age of 19 and above only. The study setting was limited to a 150 bed capacity tertiary hospital which may influence the generalizability of the study. The risk scoring was not calculated in real time during hospital admission and not used to guide clinical care.
References
- 1.Azmi Soraya. (2015) Assessing the burden of pneumonia using administrative data from Malaysia, Indonesia, and the Philippines.
- 2.Ahn Dae-Gyun. (2019) Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease.
- 3.Chakraborty C. (2020) SARS-CoV-2 causing pneumonia-associated respiratory disorder (COVID-19): diagnostic and proposed therapeutic options.
- 6.Herriman. (2018) Pneumonia is the 3rd biggest killer in the Philippines, accounting for 10 percent of deaths. http://outbreaknewstoday.com/pneumonia-3rd-biggest-killer-philippines-accounting-10-percent-deaths-91248/
- 8.PIRO.score for community-acquired pneumonia: a new prediction rule for assessment of severity in intensive care unit patients with community-acquired pneumonia.
- 12.Eguerra-Llabado Giselle. (2019) Comparative Study of CAP-PIRO Score and CURB-65 as an assessment tool to Predict Severity of Community Acquired Pneumonia among Adult patients admitted in a Tertiary Hospital. , Quezon City, PH
- 13.Pinera R. (2016) Validation of the VAP PIRO Score in predicting ICU mortality and Length of ICU stay in VAP diagnosed aptients at Veterans Memorial Medical Center. , Quezon City;
- 14.Jeffrey D Blume. (2009) Bounding Sample Size Projections for the Area Under a ROC Curve. , Journal of Statistical Planning and Inference 139-1.
- 15.P J McDonald. (2014) Comparison of PIRO, SOFA, MEDS scores for predicting mortality in emergency department patients with severe sepsis and septic shock. , Australia
- 16.Rello J. (2009) PIRO score for community-acquired pneumonia: a new prediction rule for assessment of severity in intensive care unit patients with community-acquired pneumonia. , Critical Care Medicine 37(2).